The GLP-1 Secret No One Talks About: Why Fast Weight Loss Can Leave You Tired, Weaker, and Less Healthy!
You’ve probably seen the ads — glossy, smiling faces promising effortless weight loss.
Ozempic. Wegovy. Mounjaro.
They’re everywhere! On screens, in conversations, at dinner tables.
And it’s no wonder. After decades of frustration with diets that don’t deliver, these GLP-1 medications have become the newest promise of effortless results.
For many, they truly are life-changing tools.
But as a naturopathic doctor who has spent over 14 years studying metabolism and blood work, I want to ask a question that too few people….and almost none of those glossy ads are asking:
What exactly are you losing when you lose weight this fast?
Because when the number on the scale drops, it’s not just fat leaving your body. For many, it’s muscle, and that loss can silently change the way your body functions long after the injections stop.
The GLP-1 Revolution — and Its Missing Chapter
GLP-1 receptor agonists like semaglutide and tirzepatide were first designed to help people with type 2 diabetes regulate blood sugar.
Clinical trials soon revealed a surprising side effect: dramatic weight loss.
In the landmark STEP-1 trial (New England Journal of Medicine, 2021), participants lost an average of 14.9 percent of their body weight in 68 weeks.
But inside that success story is a quieter detail: in detailed DXA body-composition studies, about 25–30 percent of the weight lost was lean mass, with the remaining 70–75 percent from fat.
That means if you lose 22 pounds, roughly five to seven pounds of it may be lean tissue.
That shift has far-reaching consequences.
Why Muscle Is the Organ of Longevity
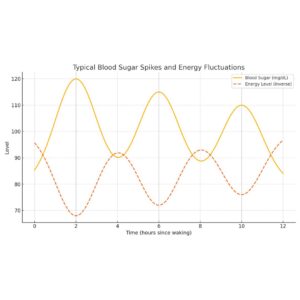
When most of us think “muscle,” we picture the gym. But muscle isn’t just about strength or tone, it’s an organ of metabolism.
At rest, each pound of muscle burns roughly six calories per day, while fat burns about two, a small difference per pound, but meaningful over time because muscle mass drives overall metabolic rate.
So when you lose muscle, your metabolism quietly slows, meaning your body now needs fewer calories just to maintain itself.
It’s like trading a roaring fire for a steady candle, still burning, but not radiating the same warmth or vitality.
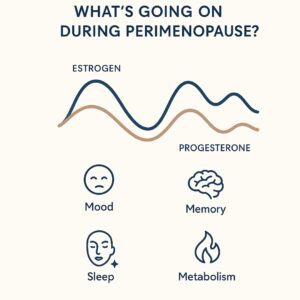
For women in their 40s, 50s, and 60s, this matters more than ever.
Hormonal changes during perimenopause and menopause accelerate muscle loss and slow recovery. Add a medication that suppresses appetite, and the risk compounds.
You burn fewer calories, your strength declines, and the moment you stop the medication or relax your routine, weight often returns, but this time, mostly as fat.
The Invisible Trade-Off
Imagine this:
You step on the scale and see you’re down 22 pounds.
You feel proud.
But under the surface, your body composition has shifted. Less muscle supporting your joints, fewer mitochondria generating energy, less strength to carry you into the next decade of your life.
That’s the piece missing from the national conversation.
Lean mass doesn’t just shape your body, it protects it. It stabilizes blood sugar, supports mood, preserves bone density, and keeps you mobile and independent as you age.
In fact, adults with higher muscle mass have significantly lower all-cause mortality, even when body weight is higher. Muscle isn’t vanity; it’s a biomarker of longevity.
So yes, GLP-1s can help you lose weight, but without protecting muscle, that “quick fix” can quietly erode the very foundation of your long-term wellness.
The Science of Strength as We Age
Starting in our 30s, we naturally lose 3–8 percent of muscle per decade.
After menopause, the decline accelerates, driven by lower estrogen, reduced growth hormone, and less physical activity.
When appetite drops or protein intake falls, that decline accelerates even more.
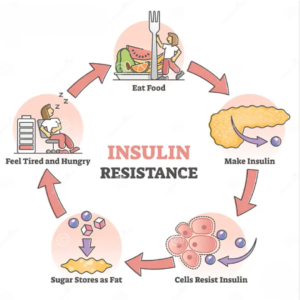
Muscle is also the body’s largest reservoir for glucose. When it shrinks, our ability to manage blood sugar worsens….ironically increasing the same metabolic stress GLP-1s were meant to help.
This is why so many patients report feeling “weaker,” “slower,” or “colder” after months on these medications. Their metabolism hasn’t just adapted, it’s down-regulated.
But here’s the good news: muscle is adaptive, too. With the right nutrition and movement, you can rebuild it , even after 60.
Beyond the Scale: Measuring What Really Matters
One of the biggest mistakes in medicine, and marketing is treating the scale as the ultimate scoreboard.
It’s not.
Your total weight says nothing about what’s actually changing inside your body.
Two people can both weigh 150 pounds: one with healthy muscle and low visceral fat, the other with little muscle and hidden inflammation. The number is identical; the health outcome is not.
That’s why, at Higher Health, we’ve invested in the InBody 380, a medical-grade body composition analyzer that measures muscle mass, fat distribution, hydration, and cellular vitality through a marker called phase angle.
DXA is the gold standard in research, but advanced analyzers like the InBody now make it possible to track muscle, fat, and hydration shifts accurately in everyday practice.
Because once you understand your data, how your body responds to nutrition, training, and recovery, you can adjust early, before small imbalances turn into bigger problems.
And this isn’t just for patients on GLP-1s. It’s for anyone who wants to understand their body beyond weight, whether you’re lifting more, eating better, or managing stress differently.
How to Protect Your Muscle While Losing Weight
If you’re using a GLP-1 medication, or considering one, you can absolutely make it part of a healthy, sustainable plan. The key is preserving muscle while reducing fat.
Here’s how:
- Eat enough protein.
Aim for 1.2–1.6 grams per kilogram of body weight per day
That’s about 90–110 grams for many women. Divide it evenly across meals — your muscles can only use so much at once. - Strength train regularly.
Resistance training two to three times per week stimulates muscle growth even during calorie restriction.
Pair this with walks or light cardio for metabolic flexibility. - Prioritize recovery.
Sleep is when growth hormone and muscle repair peak. Skimp on sleep, and you’ll lose more lean tissue. - Monitor progress with more than a scale.
A body-composition scan every three to six weeks keeps you honest about what you’re losing — and helps adjust your plan in real time. - Stay nourished.
Micronutrients like iron, B12, magnesium, and vitamin D support energy metabolism and muscle repair — especially crucial for women.
This isn’t about perfection. It’s about awareness and using every tool wisely.
Looking Ahead: From Quick Fix to Long-Term Vitality
Weight loss can be empowering. It can renew energy, confidence, and hope.
But the real goal isn’t just to weigh less, it’s to live more.
GLP-1s can be part of that journey. They can reset appetite, break patterns, and create momentum. Yet, if you focus only on the number on the scale, you miss the deeper transformation happening (or not happening) inside your body.
At Higher Health, we believe that data builds confidence. That’s why we now offer our patients complimentary body-composition tracking with the InBody 380 — especially those using GLP-1s.
You deserve to know not just how much weight you’re losing, but what kind — because real wellness isn’t measured in pounds, it’s measured in the vitality you feel every day.
Take the Next Step
At Higher Health, we believe informed care builds lasting results.
If you’re using a GLP-1 or exploring weight-loss options, book your complimentary consultation and see what your scale can’t show you, your muscle, fat, hydration, and overall vitality.
Protect your muscle. Support your metabolism.
And give your body the chance to truly thrive.
References
- Wilding J.P.H. et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384:989–1002.
- Linge J. et al. Muscle Mass and GLP-1 Receptor Agonists. Circulation. 2024.
- Look M. et al. Body Composition Changes with Tirzepatide in SURMOUNT-1. Diabetes Obes Metab. 2025.
- Karakasis P. et al. Effect of GLP-1 Receptor Agonists and Co-agonists on Body Composition: Meta-analysis of 22 RCTs. Metabolism. 2024.
- Leidy H.J. et al. Protein and Weight Management. Am J Clin Nutr. 2015.