What Is Leaky Gut And How You Can Help Fix It!
Before you get into this article, if at anytime you want to speak to one of our Toronto Naturopathic Doctors about Leaky Gut, we have a free consultation call available. Click here to book one.
If you’re reading this article, odds are you’ve been experiencing some digestive issues and may be wondering if it’s due to leaky gut syndrome. Well, you’ve come to the right place!
First, let’s start off with a quick recap about the function of how your gut lining works. Our intestines, referred to as our gut, contain specialized cells called enterocytes that line the gut wall.
The small intestine lining is a single celled mucosal layer, responsible for the absorption of water, glucose, peptides, amino acids, lipids, vitamins, and more! This lining is covered with enzymes that promote digestion, and covered in mucus that helps food and waste products make its way through the intestines.
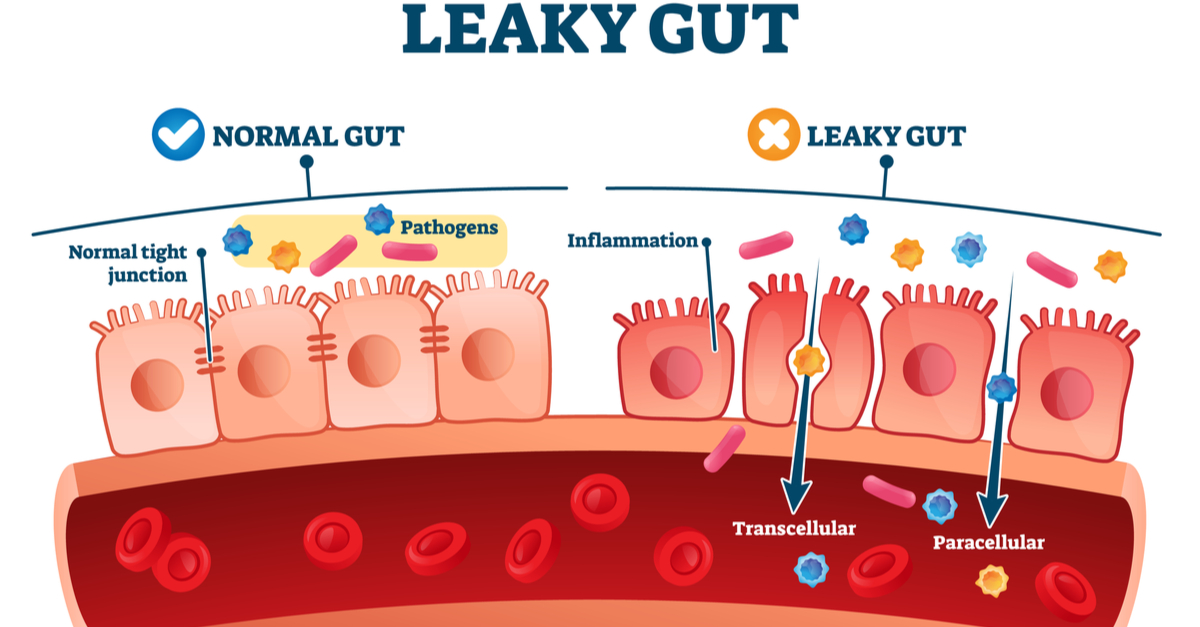
In a healthy state, your gut is extremely selective for what it is permitted to pass through and get absorbed into the bloodstream and into systemic circulation.
These gatekeepers called “tight junctions” keep the cells just that, very “tight” together. Think of them as the bodyguards of your gut, only allowing entry to those that are on the guest list.
What Is Leaky Gut?
Leaky gut, also known as intestinal permeability refers to when the gaps (tight junctions) between neighboring cells in the gut lining are disturbed. Bigger openings allow the passage of foreign substances that normally would not be allowed to pass through, this is known as the gut becoming “leaky”.
This can allow bigger molecules of undigested food, toxins, and pathogens to make their way into the bloodstream and into the body. Your body recognizes that these molecules should not be there, and this triggers an immune response and subsequent inflammation, which is linked to many inflammatory and auto-immune diseases.
What Causes Leaky Gut?
The causes of leaky gut can vary, and are often due to a variety of factors. This could include small intestinal bacterial overgrowth (SIBO), bacterial dysbiosis, food allergies or intolerances, NSAID use, stress, high intake of sugar, alcohol, or highly processed foods, or low stomach acid.
It’s important to note that leaky gut is a syndrome, and often there are a variety of contributing factors. A leaky gut has also been found to be associated and play a role in many different diseases.
What are some of the symptoms of Leaky Gut?
- Bloating
- Gas
- Diarrhea
- Constipation
- Abdominal pain
- Nutrient deficiencies
- Food sensitivities
- Fatigue
- Joint/ structural pain
- Immune issues/ dysfunction
It’s worth highlighting that you can have a leaky gut, even if no gastrointestinal symptoms are present; an individualized assessment by your Toronto Naturopathic Doctor is critical.
What are some of the diseases associated with Leaky Gut?
- Cardiovascular diseases and conditions
- Central nervous system conditions: migraines, chronic fatigue syndrome, fibromyalgia, fatigue, anxiety, depression, mood disorders
- Digestive conditions and diseases : irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), celiac disease, food sensitivities
- Immune system conditions: autoimmune disorders, recurrent or chronic infections
- Skin conditions: eczema, psoriasis, severe acne, hives
- Musculoskeletal system: rheumatoid arthritis, joint pain, muscle pain
- Respiratory system: allergies, asthma, chronic congestion, COPD
- Endocrine diseases: PCOS, type 2 diabetes
How can Toronto Naturopathic Medicine help?
It’s important to discuss diagnostic options to determine whether a leaky gut could be an underlying factor for your symptoms. Your Naturopathic Doctor can discuss what may be the best option for you to test and assess this.
In terms of gut health, Toronto Naturopathic Doctors will often talks about the 4 R’s.
Let me introduce them to you: remove, replace, repair, reinoculate! This targets the identification and removal of provocative agents that may be worsening the intestinal permeability, helps to get to root cause of its development, and also supports the healing and regeneration of the intestinal wall!
Remove:
- Eliminate potential toxic and offending foods from your diet. For example, gluten and dairy, and alcohol can damage the tight junctions in the gut.
- Avoid additives often found in pre-packaged food that can damage the gut lining (i.e. emulsifiers and stabilizers like carrageenan, polysorbate 80, and carboxymethylcellulose).
- Avoid processed and inflammatory foods such as deep fried foods and foods high in refined oils (canola, vegetable, sunflower oils), and foods high in trans fat. When possible, stick to real, whole foods.
- Identify factors contributing to stress, and discuss possible treatment strategies to manage stressors.
- IgG Food sensitivity testing may be relevant to identify any triggering foods unique to you, and to remove while allowing the gut to heal.
Replace:
- Replace gut irritating foods with foods that promote the health of your gut; bone broth is great here!
- High, easy to digest fibre rich foods that promote a healthy bacteria balance, and help to promote regularity of bowel movements (important in eliminating toxins).
- Replace processed, high-sugar, inflammatory foods with things such as fruits, vegetables, fish, and avocado/olive oil that are anti-inflammatory in nature. These foods can also help to decrease pathogenic bacteria and promote the proliferation of beneficial bacteria.
Repair:
- Supplementation: L-glutamine and zinc can help to repair the intestinal lining. Anti-inflammatories like curcumin, Boswellia and omega-3s can help reduce inflammation.
- Botanicals: Herbs like slippery elm, licorice, and marshmallow root can help protect the lining of the digestive tract.
- Continue to avoid triggering foods.
Reinoculate:
- Supplementation with probiotics specific to you and your gut health goals to ensure a well-balanced microbiome
- Continue eating a fibre-rich diet, which act as prebiotics (food for the healthy bacteria to proliferate)
- Consider adding in fermented foods that are rich in probiotics (like kimchi, kefir, sauerkraut, miso, tempeh)
As every individual is unique, your treatment plan will also be unique to you; there is no one size fits all approach. Your Toronto Naturopath will work with you to help determine whether leaky gut may be a contributing factor to your symptoms, and tailor a treatment plan accordingly to help you feel your best self!
If you have more questions about leaky guy, digestive health, or your health in general, please book a free consultation with one of our Naturopathic Doctors today.
References:
https://www.hindawi.com/journals/mi/2015/628157/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440529/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4637104/
https://www.health.harvard.edu/blog/putting-a-stop-to-leaky-gut-2018111815289
https://www.health.harvard.edu/blog/leaky-gut-what-is-it-and-what-does-it-mean-for-you-2017092212451